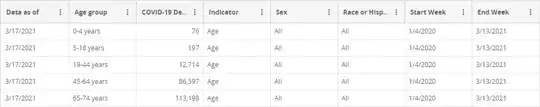
Update 2021-03-24: Based on new data through "End Week" 3/13/2021:
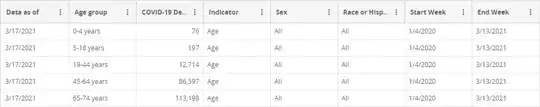
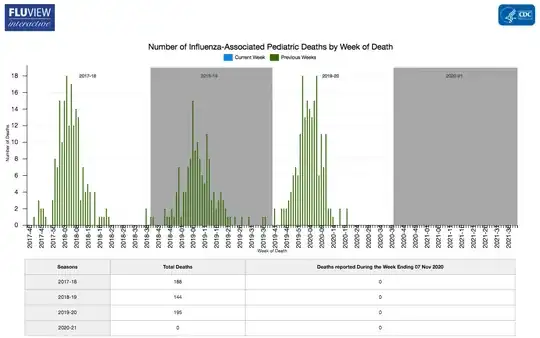
the CDC tallied total COVID-19 death toll among children since the beginning of the pandemic (which has now had meaningful cases in the U.S. for almost precisely a year) is up to 273 (76 in 0-4 range, 197 in 5-18 range). By itself, this doesn't meaningfully change the original answer (273 still falls within the 37 to 600 range where we couldn't give a definitive answer without a head-to-head comparison), but:
- It is higher than the officially reported pediatric death toll for any typical flu season (so if the rate of missed deaths was even remotely similar, more children died of COVID-19 this past year than in any typical flu season).
- The same mitigation measures (or lack thereof) have now been in place during a flu season as well, so we have one cold/flu season in which both COVID-19 and the flu were operating, and both were subject to all the same mitigations aside from vaccines (no pediatric COVID-19 vaccine has been approved yet; they've barely started testing them).
With that in mind, the new comparison is:
- COVID-19 killed 273 children in the U.S. this past year, 138 of them between early November (when the data from the original answer was pulled) and mid-March (current data at time of writing), a period encompassing the height of most flu seasons (the flu season typically extending a month further on either side, but with fewer deaths on either end).
- The flu killed one child in the U.S during this past flu season (6-9 for the past year depending on whether you start from March or April, counting deaths from the tail of the previous flu season).
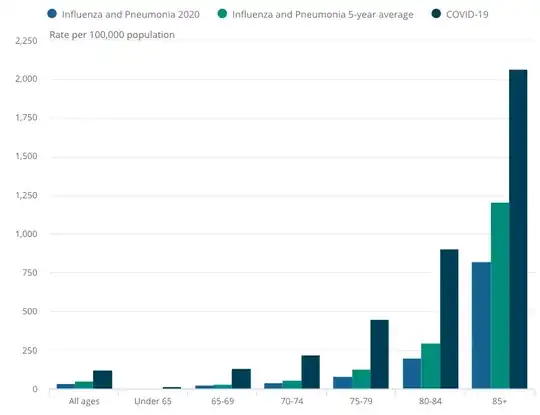
Even if we assume it was a low danger flu strain circulating this year (comparable to the one that only caused 37 pediatric deaths in a prior year), the anti-COVID-19 mitigations we made reduced the flu death toll by over 97% for this past flu season; even with inconsistent mitigations, the flu was effectively zero threat to children (the flu season basically didn't happen in either hemisphere this past year thanks to said mitigations), while COVID-19 remained a threat. So under the criteria of "which kills the most children under similar circumstances" the answer is clearly COVID-19. Even if the flu has a higher case fatality rate among children (there's no strong evidence on this either way, and it varies by strain), COVID-19 is clearly much more contagious; at any given time, your average currently uninfected child has a dramatically higher risk of dying of COVID-19 than the typical seasonal flu over the course of the following year, simply because they're far more likely to catch it, and it's lethal enough.
Original answer (still relevant for context and explanation):
"Is it true that it hit less hard on children than flu?"
Short answer up front: To the best of our knowledge, subject to the conditions we've been able to observe (vaccines for flu, lockdowns, distancing and masking for COVID-19), COVID-19 is, so far, a similar level of threat to children as typical seasonal flus; more deadly than some flu years, less deadly than others.
Long answer:
This is a hard question to answer definitively, since the death toll from the flu varies significantly from year to year. According to the CDC, the pediatric death toll from seasonal flu during the typical flu season has varied from 37 to 188 per year since 2004 (the 2009 H1N1 pandemic was an outlier, in that it had a total of 358 pediatric flu-related deaths between April 2009 to September 2010, a period of 18 months, and most of them occurred outside "typical" flu season). That said, the CDC is suspicious of the completeness of their pediatric flu death reports, and believes, based on statistical modeling, that the year with 188 deaths actually involved ~600 pediatric deaths.
If we focus on seasonal flu in general, we can say roughly, that if the annual pediatric COVID-19 death toll:
- Is below 37, then COVID-19 is less dangerous than seasonal flus
- Is between 37 and 600, then COVID-19, under existing mitigation strategies, may be less dangerous to children than some flu seasons, and probably more dangerous than others.
- Is above 600, then COVID-19 is more dangerous to children than typical seasonal flus.
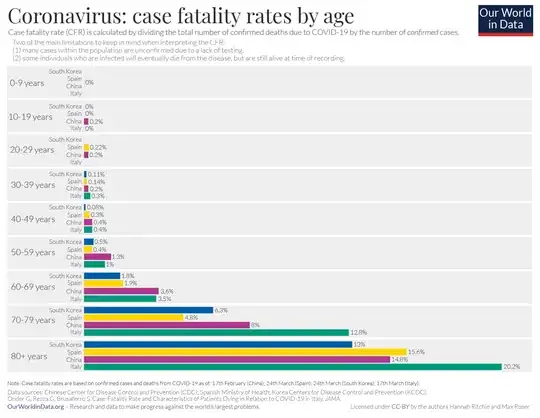
Note that this is not saying whether the child is more at risk once infected; that's much harder to determine (especially with the high rate of asymptomatic COVID-19 cases in children). If COVID-19 has a lower case fatality rate, but is sufficiently more infectious such that more children die of it, I'd argue it remains more of a threat to children than the flu for the same reason that we consider the flu a greater threat to U.S. children than we do Ebola; sure, many forms of Ebola are incredibly deadly if you catch it, but it doesn't spread easily enough to actually infect that many people under conditions in most developed countries.
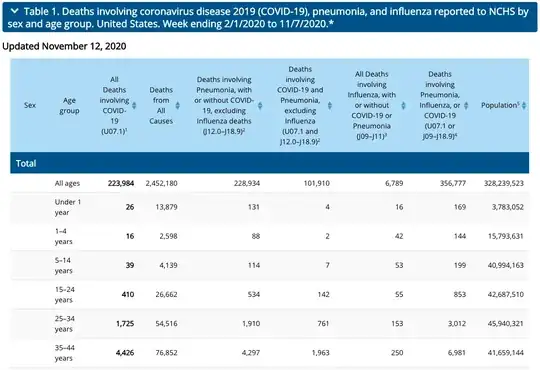
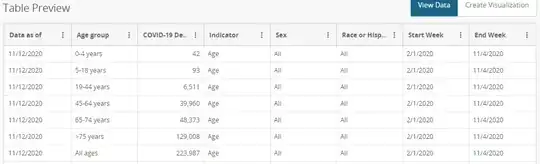
Given those bounds, based on the CDC's raw data focused on deaths aged 0-18:
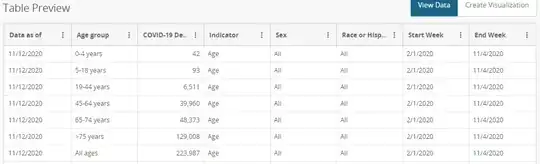
we can see that the United States has had 135 COVID-19 deaths in the 0-18 range (42 among the 0-4 group, 93 among the 5-18 group).
Thus, all we can say right now is what I said in the short answer:
To the best of our knowledge, subject to the conditions we've been able to observe, COVID-19 is, so far, of a similar level of threat to children as typical seasonal flus; more deadly than some, less deadly than others.
The qualifiers are needed because:
- With lockdowns (including school closures), masking, and distancing, we're not observing COVID-19 as it would behave "naturally" (e.g. under the "focused protection" scenario proposed by your source).
- Thanks to vaccines, we don't observe seasonal flus as they'd behave "naturally" either; approximately 80% of observed pediatric flu deaths occurred in unvaccinated or under-vaccinated (two shots are suggested the first year you receive a flu vaccine) children, even though unvaccinated children are in the minority.
- We still haven't seen how COVID-19 behaves over the course of a full cold season (Fall-Winter), which we can expect to be worse than other seasons based on the typical behavior of coronaviruses.
Issue #3 should be answerable by sometime next Spring (looking at a full year's death toll during a period where COVID-19 was fairly widespread). But #1 and #2 are harder to account for.
Pediatric flu vaccination rates in the 2017-2018 flu season (when 188 pediatric flu deaths were reported, and 600 estimated) were 57.9% overall (higher for 6 mo.-4 y.o. groups, lower for teens), and given ~80% of deaths typically occur in the unvaccinated group, one could reasonably assume the flu would kill significantly more children if the vaccine did not exist. Beyond that, lack of a vaccine would increase the number of infected individuals spreading the flu, thereby increasing the number of cases, so it's not as simple as just applying the death rate from the unvaccinated group to the vaccinated group to estimate overall death toll, you'd have to guess at how much more community spread you'd see without the vaccine.
Similarly, while there is no vaccine for COVID-19, it does appear that mitigation (lockdowns, distancing, masking) reduced COVID-19 spread (and masking in particular appears to reduce severity as well), so it's nearly impossible to state with certainty how many more children would have died from COVID-19 if we'd just ignored it and gone about our lives.