Yes.
That is: They can cause hearing loss. They are properly classified as ototoxic agents.
Paracetamol/Acetaminophen is certainly not entirely harmless. In fact it is properly classified as an ototoxic drug. An effect observed for quite some time. According to the individual studies: This is more pronounced when using it in each of these cases: higher doses, over longer time, abuse, drug combinations. But also being a women, being a man, being a kid, being elderly. If that sounds paradoxical, be aware that most studies do not even look at the general population but only subgroups, restricting their outcomes to the subgroup studied.
Of these, analgesic drug combinations seem to be the most risky, followed directly by combination with any other ototoxic drug.
However, this is also not peculiar for paracetamol alone, as aspirin for example can have this effect as well. The models to explain this effect are convincing, but real life outcome measures and population risk quantification remain a bit lacking for now.
Focusing on paracetamol: it is an ototoxic chemical, the possible mechanisms quite clearly demonstrated. Then dosage makes the poison, and neither observational long term studies in sufficient quantity and quality are available, nor are human experiments or prospective studies on that level available.
Over-the-counter painkillers linked to hearing loss. The three most commonly used medications in the U.S. have a significant, and little known, side effect.
Ototoxicity is a trait shared by several classes of drugs,
most notably by aminoglycoside antibiotics, cisplatin chemotherapy and by acetaminophen combined with narcotic medication. Animal models help to elucidate the mechanisms of hearing loss from these medications.
Acetaminophen combined with narcotic medications, when taken chronically at acceptable doses or when abused at high doses, causes profound irreversible sensorineural hearing loss. Hearing loss had previously only been reported after the use of the narcotic propoxyphene. For this reason it was initially believed that the narcotic in Lortab! (Whitby Pharmaceuticals, Richmond, VA) or Vicodin! (Abbott Laboratories, Abbott Park, Illinois, USA) was responsible for the ototoxicity. However, research in mouse auditory cell line and cochlea cultures show that of the two active ingredients in these drugs, acetaminophen, and not hydrocodone, is responsible for hair cell toxicity. Curhan et al. recently published a study examining the incidence and hazard ratio of self-reported hearing loss due to regular use of aspirin, other NSAIDs and acetaminophen. They reviewed reports in 26,917 men aged 40–74 years, with baseline hearing at 1986, and found 3,488 incident cases of hearing loss. For NSAIDs and acetaminophen, the risk increased with longer duration of use. The hazard ratio for acetaminophen was 1.22, and in men < 50 years old the risk increased to 1.99, more than the other drugs.
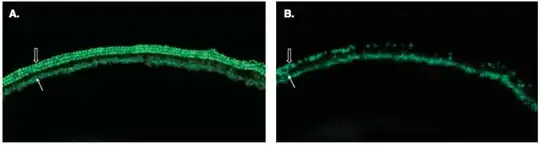
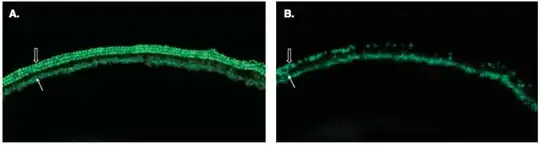
Figure 2. Fluorescent microscopy of the basal turn of the cochlea in a control culture (A) with Math1-GFP fluorescence demonstrating the intact single row of inner hair cells (closed arrow) and three rows of outer hair cells (open arrow). A basal turn of a culture exposed to high-dose acetaminophen (B) with decreased Math1-GFP expression demonstrating damage of inner (closed arrow) and outer hair cells (open arrow) compared to the control culture.
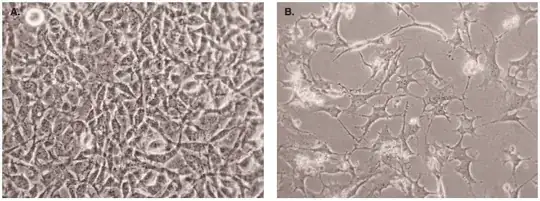
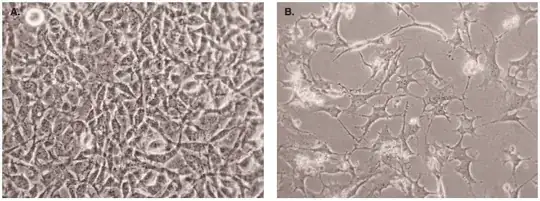
Figure 3. Light microscopy of HEI-OC1 cells in culture after 48 h when exposed to hydromorphone alone (A) compared to hydromorphone and acetaminophen (B).
–– Joshua G Yorgason†, William Luxford & Federico Kalinec: "In vitro and in vivo models of drug ototoxicity: studying the mechanisms of a clinical problem", Expert Opinion on Drug Metabolism & Toxicology, Volume 7, Issue 12, 2011.
Kalinec GM et al.: "Acetaminophen and NAPQI are toxic to auditory cells via oxidative and endoplasmic reticulum stress-dependent pathways", Hear Res. 2014 Jul;313:26-37. doi: 10.1016/j.heares.2014.04.007. Epub 2014 Apr 30.
Yorgason JG, Kalinec GM, Luxford WM, et al.: "Acetaminophen ototoxicity after acetaminophen/hydrocodone abuse: evidence from two parallel in vitro mouse models", Otolaryngol Head Neck Surg 2010;142(12):814-19; 9 e1-2.
Blakley BW, Schilling H.: "Deafness associated with acetaminophen and codeine abuse", J Otolaryngol Head Neck Surg 2008;37(4):507-9.
Friedman RA, House JW, Luxford WM, et al.: "Profound hearing loss associated with hydrocodone/acetaminophen abuse", Am J Otol 2000;21(2):188-91.
Ho T, Vrabec JT, Burton AW.: "Hydrocodone use and sensorineural hearing loss", Pain Physician 2007;10(3):467-72.
Oh AK, Ishiyama A, Baloh RW: "Deafness associated with abuse of hydrocodone/acetaminophen", Neurology 2000;54(12):2345.
Lin BM, et al.: "Long-Term NSAIDs and Acetaminophen Linked to Hearing Loss in Women", Am J Epidemiol 2017;185(1): 40-7.
Zolot J: "Long-Term NSAIDs and Acetaminophen Linked to Hearing Loss in Women", Am J Nurs. 2017 Apr;117(4):16. doi: 10.1097/01.NAJ.0000515218.30710.2c.
Lin BM, Curhan SG, Wang M, Eavey R, Stankovic KM, Curhan GC.: "Duration of Analgesic Use and Risk of Hearing Loss in Women", Am J Epidemiol. 2017 Jan 1;185(1):40-47. doi: 10.1093/aje/kww154. Epub 2016 Dec 14.
McGill MR, Kennon-McGill S, Durham D, Jaeschke H.: "Hearing, reactive metabolite formation, and oxidative stress in cochleae after a single acute overdose of acetaminophen: an in vivo study", Toxicol Mech Methods. 2016 Feb;26(2):104-11. doi: 10.3109/15376516.2015.1122136. Epub 2016 Mar 16.
Novac A, Iosif AM, Groysman R, Bota RG.: "Implications of Sensorineural Hearing Loss With Hydrocodone/Acetaminophen Abuse", Prim Care Companion CNS Disord. 2015 Sep 10;17(5). doi: 10.4088/PCC.15br01809. eCollection 2015.
Joo Y, Cruickshanks KJ, Klein BEK, Klein R, Hong O, Wallhagen M.: "The Contribution of Ototoxic Medications to Hearing Loss among Older Adults", J Gerontol A Biol Sci Med Sci. 2019 Jul 8. pii: glz166. doi: 10.1093/gerona/glz166. [Epub ahead of print]
The overall data varied, demonstrating a measurable effect on self-reported symptoms from NSAIDs as a class, ibuprofen, and acetaminophen, but there are no audiometric data to confirm or refute this suggested effect. Sulindac was the only specific agents to have been studied with formal audiometry as a primary outcome in a randomized double-blind placebo-controlled trial, and the significant effect seen in the unadjusted analysis dissipated in the adjusted multivariate regression.
–– Kyle ME, Wang JC, Shin JJ.: "Impact of nonaspirin nonsteroidal anti-inflammatory agents and acetaminophen on sensorineural hearing loss: a systematic review", Otolaryngol Head Neck Surg. 2015 Mar;152(3):393-409. doi: 10.1177/0194599814564533. Epub 2015 Jan 5.
Regular use of aspirin, NSAIDs, or acetaminophen increases the risk of hearing loss in men, and the impact is larger on younger individuals.
–– Curhan SG, Eavey R, Shargorodsky J, Curhan GC.: "Analgesic use and the risk of hearing loss in men", Am J Med. 2010 Mar;123(3):231-7. doi: 10.1016/j.amjmed.2009.08.006.
Conclusion
There are several pathways and a multitude of observational data points that in vitro explain and in vivo record paracetamol as being damaging to hearing in principle. Neither really large and conclusive prospective studies are there to present seemingly exact numbers. The fact that paracetamol is swallowed by millions of people daily indicates that in doses small enough to not exceed recommended values these really long term effects are probably statistically significant, but not exceedingly strong. The risks for individuals or on the population level are to be considered separately.
The current studies looking at humans in large numbers have several weaknesses that need addressing. Self-reported hearing-loss, self-reported dose regimen over a long time span, etc. Hearing gets worse as we age, and some amount of hearing loss is 'natural' and thus unavoidable. Not all confounding factors like noise exposure, inflammation, other toxins can be properly and rigorously controlled for over such a long term.
Nevertheless, hearing loss is a very widespread problem and it looks like longterm painkiller use in moderate amounts seems to be a factor not to be overlooked in future studies. According to the observational studies in humans the current perspective is:
“Although the magnitude of higher risk of hearing loss with analgesic use was modest, given how commonly these medications are used, even a small increase in risk could have important health implications. Assuming causality, this would mean that approximately 16.2 percent of hearing loss occurring in these women could be due to ibuprofen or acetaminophen use,” said Curhan.
–– Haley Bridger: "Longer use of pain relievers tied to hearing loss in women", The Harvard Gazette, December 14, 2016.
And
For acetaminophen, regular users aged less than 50 were 99% more likely, regular users aged 50–59 were 38% more likely, and those aged 60 and older were 16% more likely to have hearing loss than non-regular users of acetaminophen. (Curhan 2010)
To turn this perspective around: The risk for any individual taking paracetamol to actually develop hearing problems from that is not expressed in the above numbers and it cannot be calculated from the numbers given so far.