Summary
The estimation of prevalence of lactose intolerance may be too high because of:
- surveys in which they included individuals with self-diagnosed and not just officially diagnozed lactose intolerance
- false positive diagnostic tests (up to 20% according to American Family Physician) due to other problems, such as irritable bowel syndrome, sensitivity to A1 milk protein, etc.
So, lactose intolerance may be wrongly diagnosed in 20% of cases, but not likely in "most" cases and even those 20% are from a variety of problems, not just from sensitivity to A1 milk protein.
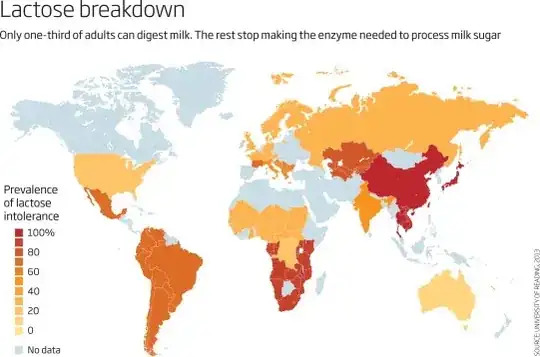
The geographical distribution of lactose intolerance and A2 (A1-free) milk
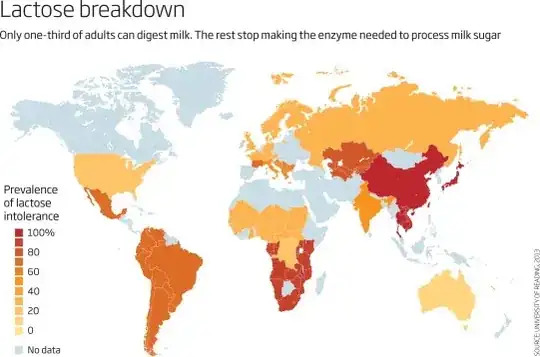
Image: Geographical distribution of lactose intolerance (source: New Scientist, 2015)
The distribution of A1 and A2 milk are from Today's Dietitian, 2017:
According to the California Dairy Research Foundation, the typical
dairy cow in the United States produces approximately equal amounts of
A1 and A2 forms of beta-casein in its milk. Dairy herds in much of
Asia and Africa and parts of Southern Europe are naturally more likely
to produce only A2 proteins.
So, in the areas with cows with A1-free (A2-only) milk (Asia, Africa, South Europe), the estimated prevalence of lactose intolerance is high, which does NOT support the hypothesis that it is sensitivity to A1 milk that causes gastrointestinal problems in most individuals diagnosed with lactose intolerance.
A1 vs A2 milk and gastrointestinal symptoms
In few studies reviwed here Systematic Review of the Gastrointestinal Effects of A1 Compared with A2 β-Casein (Advences in Nutrition, 2017), consumption of A1 milk was associated with gastrointestinal symptoms in some individuals, but the prevalence of the problem is not known:
In humans, there is evidence from a limited number of studies that A1
consumption is also associated with delayed intestinal transit (1
clinical study) and looser stool consistency (2 clinical studies). In
addition, digestive discomfort is correlated with inflammatory markers
in humans for A1 but not A2. Further research is required in humans to
investigate the digestive function effects of A1 relative to A2 in
different populations and dietary settings.
Lactose intolerance
In people with lactose intolerance, lactose is not fully digested due to lack of the enzyme lactase in the small intestinal lining. The undigested lactose is ultimately fermented by normal large intestinal bacteria, which produce gas and thus cause bloating and flatulence.
Hydrogen breath test for lactose intolerance:
The diagnosis of lactose intolerance is made by a hydrogen breath test in which you drink 25-50 grams of lactose in water solution (to compare: ~50 g lactose is in 1 liter of milk) and if you can't digest lactose, it will be fermented by intestinal bacteria, which will produce hydrogen, which will be absorbed into the blood and appear in your breath (intestinal bacteria are the only source of hydrogen that appears in breath). However, the test does not confirm the actual lack of the enzyme lactase, so it can be positive in other conditions with malabsorption and increased intestinal motility, in which lactose travels fast through the intestine and does not have time to be digested, for example, due to psychological expectation of intolerance, irritable bowel syndrome, small intestinal bacterial overgrowth, fructose malabsorption, celiac disease, Crohn's disease, etc (American Family Physician, 2002, Monash University, 2018). This means, it's likely that lactose intolerance is overdiagnosed, but we can't say by how much.
Individuals who are positive after a 25 g lactose test are said to be "high-grade malabsorbers." Anyway, in one 2008 study, only 16 out of 90 adults diagnosed as high-grade malabsorbers were positive after the test using 12.5 g lactose (which can be found in 1 cup or 244 g of milk).
Lactose intolerance prevalence:
Science Daily, 2009:
Previous studies have found lactose maldigestion, or low lactase
activity in the gut, to occur in approximately 15 percent of
European Americans, 50 percent of Mexican Americans and 80 percent of
African Americans.
Nutrition Today, 2009:
However, lactose-intolerance prevalence rates in practical life
settings may be lower than originally suggested. The goal of this
study was to determine the prevalence of self-reported lactose
intolerance among a national sample of European American (EA), African
American (AA), and Hispanic American (HA) adults. Interviews were
completed by a total of 1,084 respondents between the ages of 19 and
70 years with 486 EAs, 355 AAs, and 243 HAs. The age-adjusted
lactose-intolerance prevalence estimates were 7.72%, 19.50%, and
10.05% for EAs, AAs, and HAs, respectively. For all respondents in the sample, the crude and age-adjusted self-reported lactose-intolerance
prevalence rates were 13.38% and 12.04%, respectively.
So, the old vs new 2009 estimation of lactose intolerance prevalence in Americans is:
- All Americans: 15-30% vs 13%
- European Americans: 15% vs 8%
- African Americans: 80% vs 20%
- Mexican (Hispanic) Americans: 50% vs 12%
Conclusion
High estimates of lactose intolerance prevalence my be due to:
- Large amounts of lactose used in hydrogen breath tests (up to 50 g, which is equivalent of 1 liter of milk)
- False-positive test results due to:
- personal differences in how fast lactose travels through the gut
- other problems, like iritable bowel syndrome (but not mainly due to sensitivity to A1 milk) or wrongly self-diagnosed lactose intolerance